Life-Changing Comprehensive Guide to Pancreatic Cancer Treatment
Introduction to Pancreatic Cancer
Pancreatic cancer, a malignancy originating in the tissues of the pancreas, is notoriously challenging to diagnose and treat. It often progresses rapidly and is frequently discovered in advanced stages, making early detection and effective treatment paramount. This guide provides an in-depth exploration of pancreatic cancer, focusing on state-of-the-art treatments, emerging therapies, and holistic management strategies.
Understanding Pancreatic Cancer
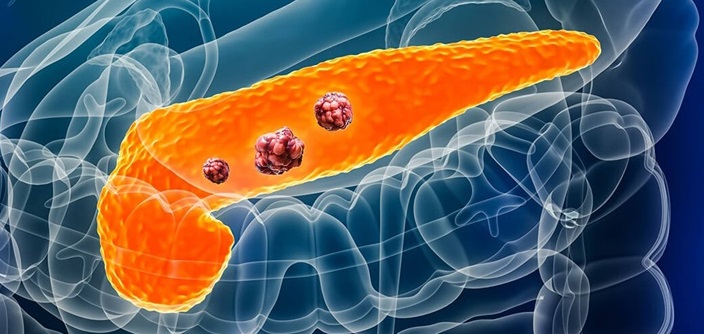
What is Pancreatic Cancer?
Pancreatic cancer develops in the pancreas, an organ situated behind the lower part of the stomach. The pancreas plays a crucial role in digestion and blood sugar regulation. The cancer can start in the exocrine cells that produce digestive enzymes or in the endocrine cells that produce hormones, such as insulin.
Types of Pancreatic Cancer
- Exocrine Tumors: The most common type, including adenocarcinomas.
- Endocrine Tumors: Also known as pancreatic neuroendocrine tumors (NETs), these are less common but tend to have a better prognosis.
Symptoms and Diagnosis
Symptoms
Pancreatic cancer symptoms are often subtle and non-specific, leading to delayed diagnosis. Key symptoms include:
- Jaundice (yellowing of the skin and eyes)
- Unexplained weight loss
- Persistent abdominal or back pain
- Loss of appetite
- Nausea and vomiting
- New-onset diabetes or worsening of existing diabetes
Diagnostic Procedures
Early detection is critical for improving outcomes. The following diagnostic tools are used:
- Imaging Tests: CT scans, MRI, and endoscopic ultrasound (EUS) to visualize the pancreas.
- Biopsy: Obtaining tissue samples through EUS-guided fine-needle aspiration.
- Blood Tests: Checking for tumor markers such as CA 19-9.
Treatment Options
Surgery
Surgery offers the best chance for a cure in localized pancreatic cancer. Surgical options include:
- Whipple Procedure (Pancreaticoduodenectomy): Removes the head of the pancreas, part of the small intestine, the gallbladder, and a portion of the bile duct.
- Distal Pancreatectomy: Removes the body and tail of the pancreas.
- Total Pancreatectomy: Removes the entire pancreas and is less commonly performed.
Radiation Therapy
Radiation therapy uses high-energy rays to target and kill cancer cells. It can be used before surgery to shrink tumors, after surgery to eliminate residual cancer cells, or as a palliative treatment to relieve symptoms.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. It can be administered orally or intravenously and is often used in combination with radiation therapy. Common chemotherapy regimens include:
- FOLFIRINOX: A combination of fluorouracil, leucovorin, irinotecan, and oxaliplatin.
- Gemcitabine: Often combined with other drugs like nab-paclitaxel.
Targeted Therapy
Targeted therapy involves drugs that specifically target cancer cell mechanisms. For pancreatic cancer, this might include drugs targeting specific genetic mutations or cellular pathways.
Immunotherapy
Immunotherapy leverages the body’s immune system to fight cancer. While not yet a standard treatment for pancreatic cancer, clinical trials are exploring its potential.
Emerging Treatments
Research is ongoing to discover more effective treatments for pancreatic cancer. Some promising areas include:
- Personalized Medicine: Tailoring treatment based on genetic profiling of the tumor.
- New Drug Development: Investigating novel drugs and drug combinations.
- Vaccine Therapy: Developing vaccines that trigger the immune system to attack cancer cells.
Holistic and Supportive Care
Nutritional Support
Proper nutrition is essential for patients undergoing treatment. Nutritional counseling can help manage side effects and maintain strength.
Pain Management
Effective pain management is critical for maintaining quality of life. This may involve medications, nerve blocks, or alternative therapies like acupuncture.
Psychological Support
Coping with pancreatic cancer can be emotionally challenging. Access to psychological support, counseling, and support groups can provide significant benefits.
Conclusion
Pancreatic cancer remains a formidable challenge in oncology, but advancements in treatment and early detection offer hope. A multidisciplinary approach, combining surgery, chemotherapy, radiation, and emerging therapies, is essential for optimizing outcomes. Comprehensive care, including nutritional, pain, and psychological support, plays a crucial role in the holistic management of patients.
By staying informed about the latest developments in pancreatic cancer treatment, patients and caregivers can make more empowered decisions and seek the best possible care.